Introduction
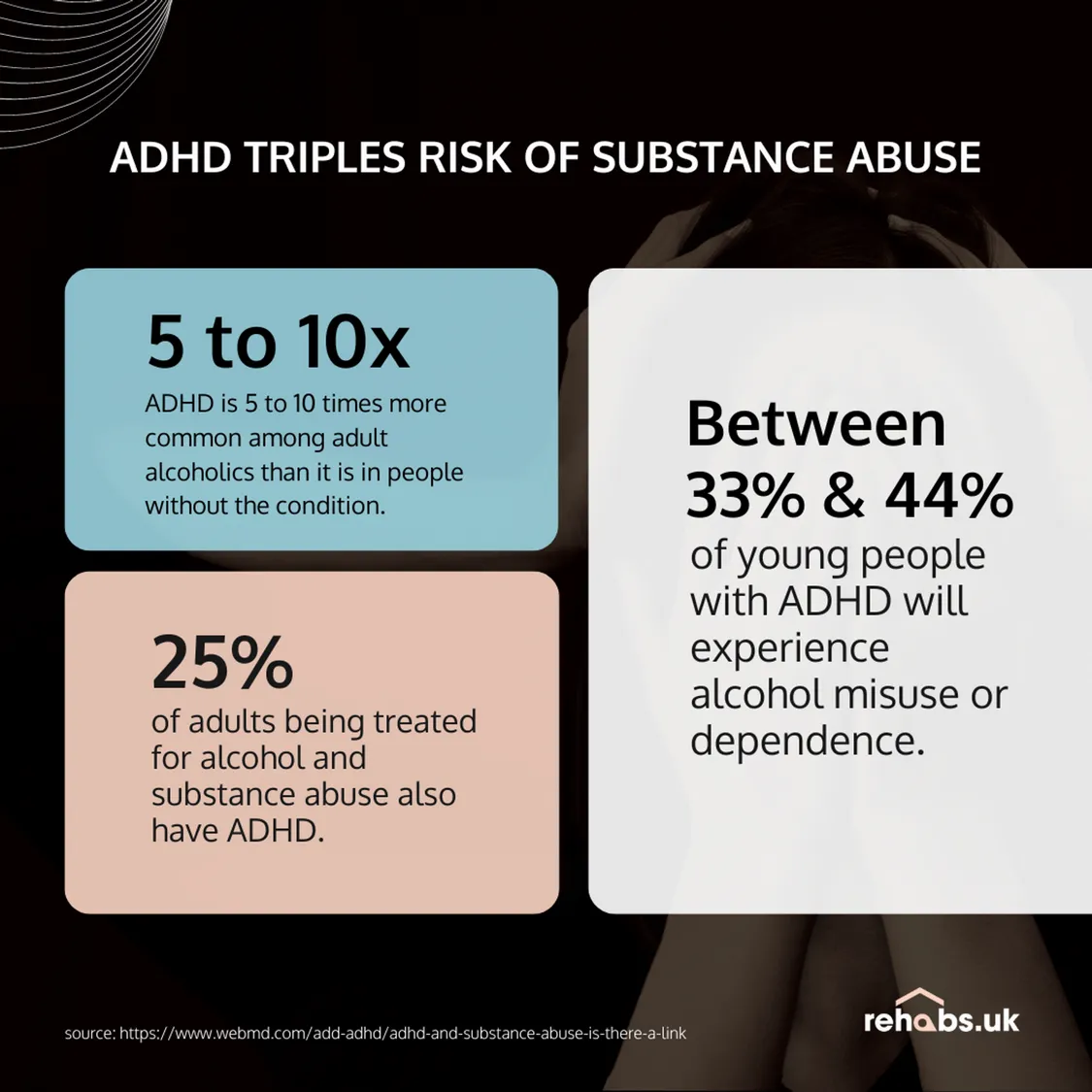
Attention-Deficit/Hyperactivity Disorder (ADHD) is often misunderstood as a childhood condition marked by restlessness or difficulty focusing. In reality, ADHD is a lifelong neurodevelopmental disorder that significantly affects how the brain processes reward, motivation, and self-control. These same brain systems are deeply involved in addiction—making people with ADHD far more vulnerable to substance use disorders.
Research consistently shows that individuals with ADHD are two to three times more likely to develop addiction compared to those without ADHD. Understanding why this risk is higher is a crucial step toward prevention, early intervention, and effective recovery.
The Dopamine Connection: A Brain Wired for Risk
Image caption: Both ADHD and addiction involve disruptions in the brain’s dopamine-based reward system.
At the core of ADHD lies a dysfunction in the brain’s dopamine system. Dopamine is the chemical responsible for pleasure, motivation, focus, and reward. In ADHD brains, dopamine activity tends to be lower or less efficient—leading to chronic understimulation.
Substances such as alcohol, nicotine, stimulants, or opioids temporarily increase dopamine levels. For someone with ADHD, this can feel like instant relief: clearer focus, calmer thoughts, emotional regulation. Unfortunately, the brain quickly learns to rely on substances for this effect, paving the way for addiction.
Impulsivity and Poor Inhibitory Control
Image caption: Impulsivity in ADHD can lead to experimentation and difficulty stopping once substance use begins.
Impulsivity is a hallmark symptom of ADHD. It affects decision-making, risk assessment, and the ability to pause before acting. This makes people with ADHD more likely to:
-
Experiment with substances at a younger age
-
Use higher quantities
-
Struggle to stop once use becomes harmful
Addiction thrives where impulse control is weak. Without strong internal “brakes,” the path from casual use to dependence becomes dangerously short.
Emotional Dysregulation and Self-Medication
Image caption: Many individuals with ADHD use substances to cope with emotional pain, stress, or overwhelm.
People with ADHD often experience intense emotions—frustration, shame, anxiety, boredom, or rejection sensitivity. These feelings can be overwhelming and difficult to regulate.
Substances are frequently used as a form of self-medication:
-
Alcohol to quiet racing thoughts
-
Nicotine to improve focus
-
Drugs to escape emotional pain
While this may offer temporary relief, it ultimately worsens emotional regulation and deepens dependency.
Earlier Onset, Faster Progression
Image caption: ADHD is associated with earlier substance use and faster progression to addiction.
Studies show that individuals with ADHD often begin using substances earlier than their peers. Early exposure interferes with brain development—especially in areas responsible for judgment and self-control—making addiction more severe and harder to treat later in life.
ADHD and Addiction: A Treatable Combination
The increased addiction risk associated with ADHD is not a life sentence. When ADHD is properly diagnosed and treated, the likelihood of developing substance use disorders drops significantly.
Effective strategies include:
-
Evidence-based ADHD treatment (behavioral therapy, medication when appropriate)
-
Trauma-informed care
-
Skills training for emotional regulation and impulse control
-
Structured routines and support systems
Recovery outcomes improve dramatically when ADHD is addressed alongside addiction—not ignored.
Conclusion
ADHD doesn’t cause addiction, but it creates a brain environment where addiction can take root more easily. Dopamine dysregulation, impulsivity, emotional overwhelm, and early exposure form a powerful risk combination.
By recognizing this connection, we can replace stigma with understanding—and shift from punishment to prevention, from relapse to resilience.