Introduction
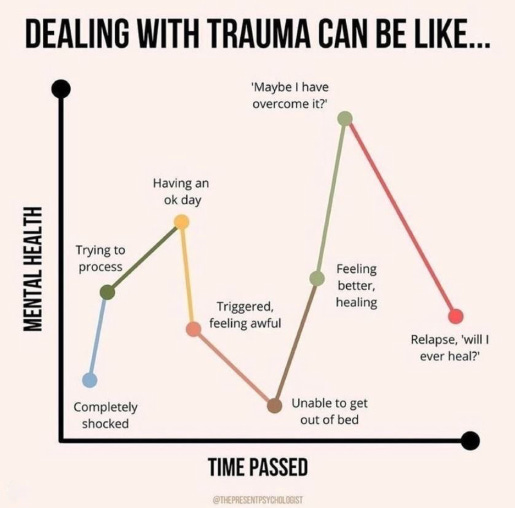
Recovery from addiction is not only about resisting substances—it’s about navigating the mind. For many people in recovery, flashbacks are one of the most dangerous and underestimated triggers for relapse. These sudden, vivid re-experiences of past trauma can overwhelm the nervous system, flood the brain with stress hormones, and reignite cravings that feel impossible to resist.
Understanding how flashbacks work—and why they increase relapse risk—is a critical step toward long-term recovery.
What Are Flashbacks?
Flashbacks are intense, involuntary memories where a person feels as if a traumatic event is happening again—right now. They are not just thoughts or memories; they involve the body, emotions, and senses.
During a flashback, a person may experience:
-
Racing heart or shortness of breath
-
Sudden fear, panic, or shame
-
Physical tension or freezing
-
Dissociation or feeling “not present”
The brain temporarily loses its sense of time, reacting as if the danger is real and immediate.
Why Flashbacks Increase the Risk of Relapse
Flashbacks create a perfect storm for relapse because they activate the same systems that addiction once soothed.
1. Overwhelming Emotional Pain
Flashbacks bring back raw emotions—terror, grief, helplessness—that feel unbearable. Substances may resurface as a familiar escape.
2. Nervous System Overload
Trauma puts the body into fight-or-flight mode. Alcohol or drugs can seem like the fastest way to shut that alarm off.
3. Loss of Rational Control
During a flashback, the prefrontal cortex (decision-making) goes offline, while survival instincts take over—making impulsive relapse more likely.
4. Learned Coping Patterns
If substances were once used to survive trauma, the brain remembers that association under stress.
Flashbacks vs. Cravings: How They Interact
Flashbacks don’t just cause cravings—they amplify them.
-
Trauma activates stress hormones (cortisol, adrenaline)
-
Stress suppresses dopamine regulation
-
The brain demands fast relief
-
Cravings spike intensely and suddenly
This is why relapse after a flashback often feels “automatic” rather than planned.
Warning Signs: When a Flashback Is Leading Toward Relapse
Recognizing early signals can prevent a setback:
-
Sudden urge to numb emotions
-
Thoughts like “I can’t handle this”
-
Isolating or withdrawing from support
-
Romanticizing past substance use
-
Feeling emotionally younger or powerless
These are not failures—they are signals that trauma is speaking.
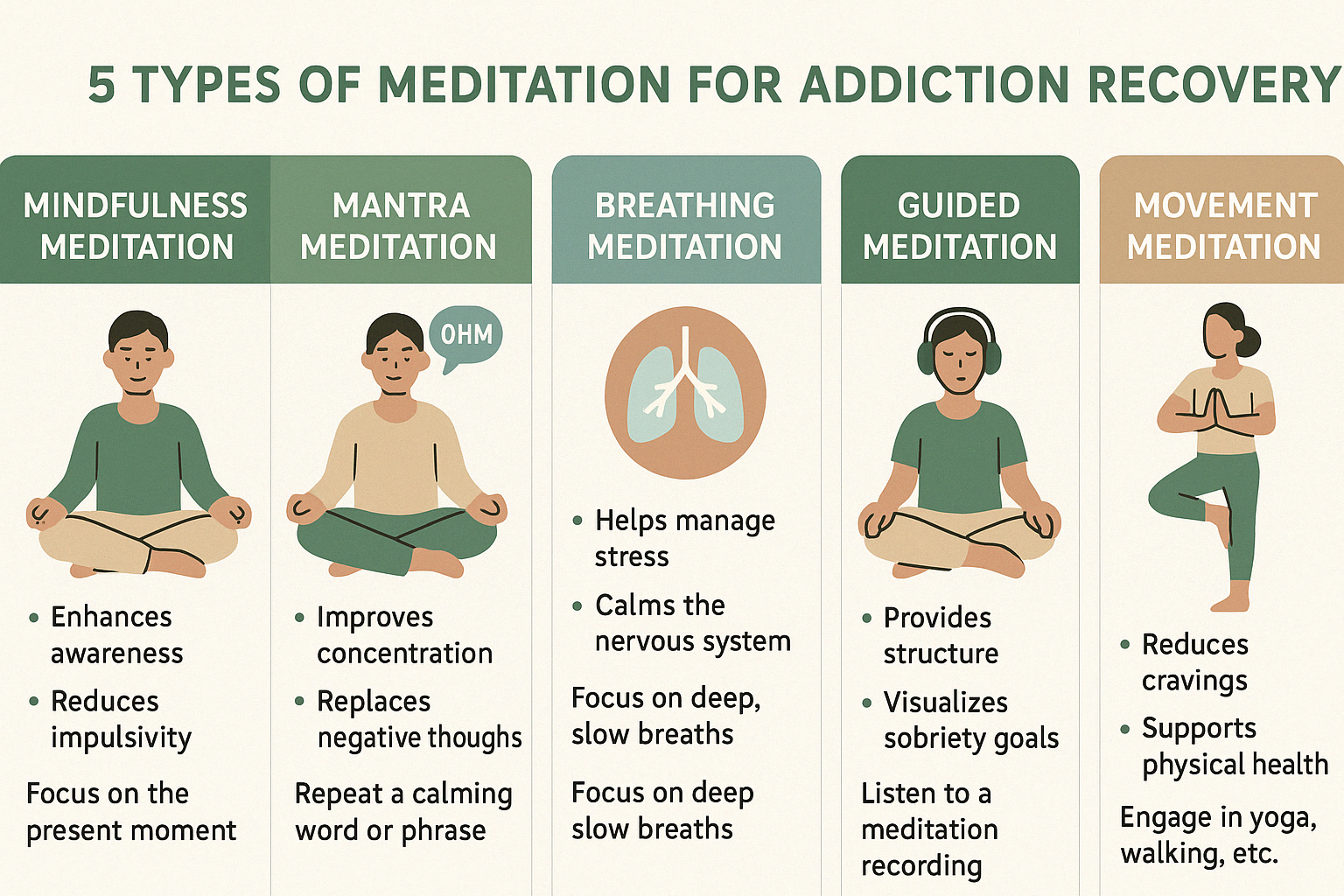
How to Reduce Relapse Risk During Flashbacks
1. Grounding Techniques
Simple actions—naming five things you see, touching a cold surface, focusing on breath—can bring the brain back to the present.
2. Trauma-Informed Therapy
Approaches like EMDR, somatic therapy, and trauma-focused CBT help retrain the brain’s response to memory triggers.
3. Build a Flashback Plan
Prepare in advance: who to call, what to do, where to go when flashbacks hit.
4. Reduce Shame
Flashbacks are symptoms, not weaknesses. Shame increases relapse risk; compassion reduces it.
5. Strengthen Safe Connections
Supportive relationships calm the nervous system and restore a sense of safety.
Recovery Is Not Just Sobriety—It’s Safety
Relapse prevention isn’t only about willpower. For trauma survivors, it’s about helping the brain learn that the danger is over.
When flashbacks are understood and treated, their power fades—and recovery becomes not just possible, but sustainable.
Final Thought
Healing trauma doesn’t erase the past—but it frees the future.
If flashbacks are part of your recovery journey, you are not broken. Your brain learned to survive—and now it can learn to feel safe again.