Introduction
Post-Traumatic Stress Disorder (PTSD) is more than painful memories or sudden flashbacks—it deeply alters how the brain responds to stress, emotions, and reward. For many people living with PTSD, substance cravings are not about seeking pleasure, but about escaping overwhelming internal pain. Understanding how PTSD triggers substance cravings is a critical step toward compassionate treatment and lasting recovery.
How Trauma Rewires the Brain
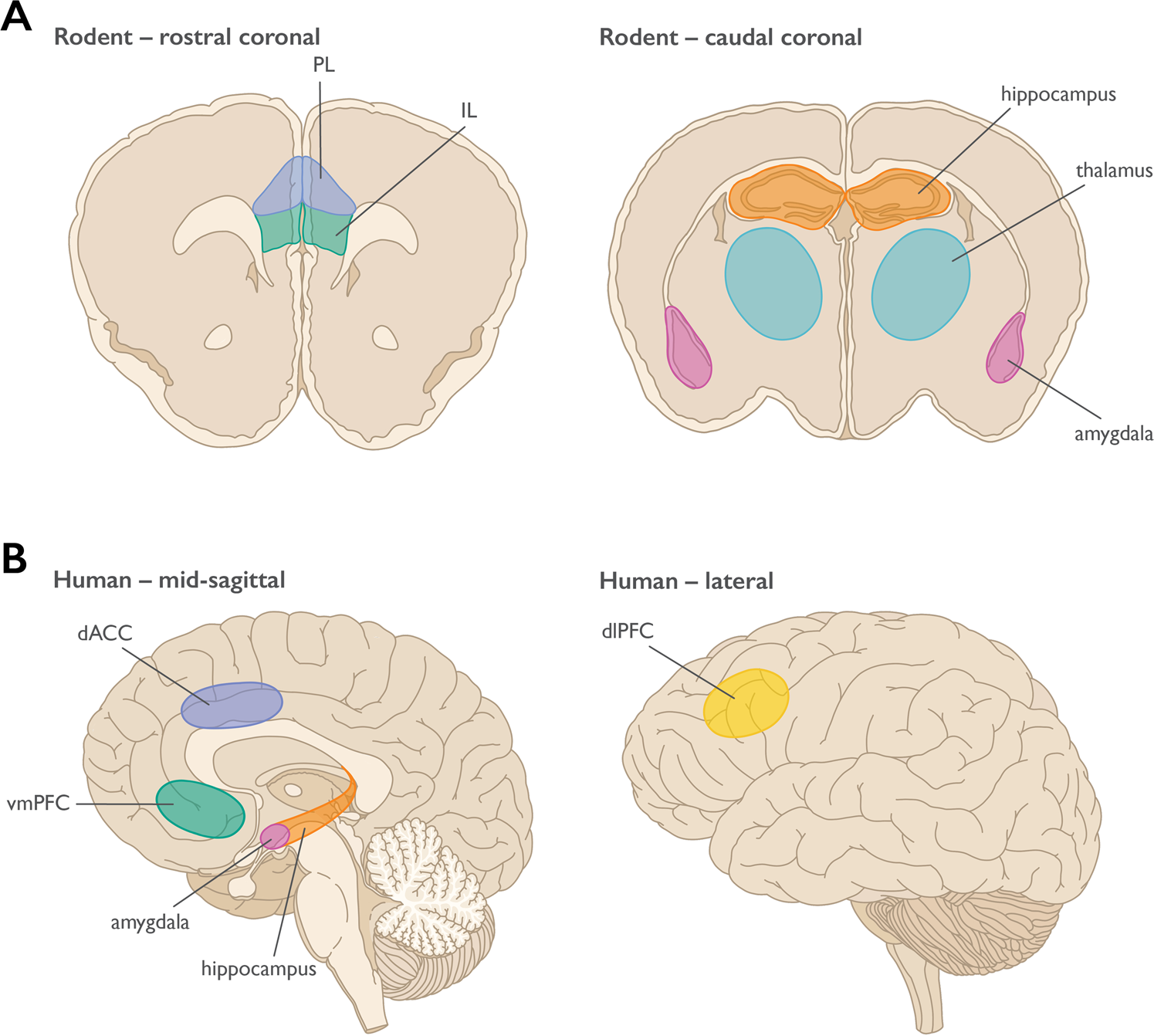
Traumatic experiences can fundamentally change the brain’s survival system:
-
Amygdala (fear center) becomes overactive, constantly scanning for danger
-
Prefrontal cortex (decision-making) struggles to regulate impulses
-
Reward system (dopamine pathways) becomes dysregulated
As a result, the brain remains stuck in “survival mode,” making relief—no matter how temporary—feel urgent and necessary.
Image caption: Trauma alters brain regions responsible for fear, impulse control, and reward processing.
Why PTSD Intensifies Substance Cravings
Substance cravings in PTSD are often state-dependent, meaning they appear when the nervous system is triggered.
1. Substances as Emotional Numbing Tools
Alcohol, opioids, nicotine, or stimulants may temporarily:
-
Reduce hyperarousal
-
Numb intrusive thoughts
-
Quiet emotional pain
The brain learns to associate substances with “safety” or “relief,” reinforcing cravings.
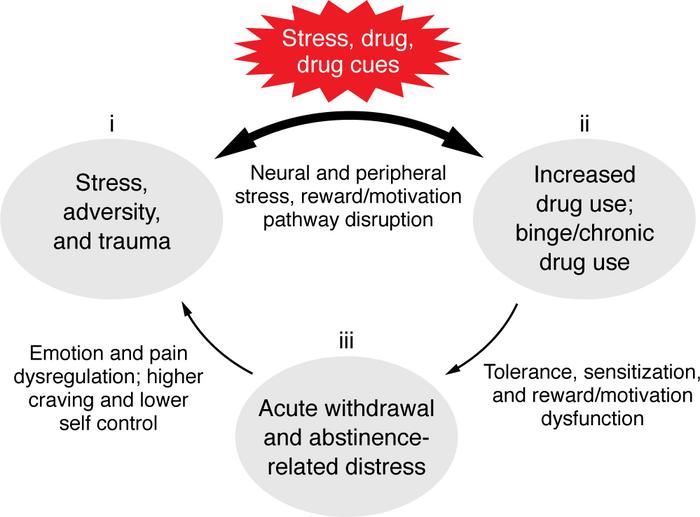
2. Triggers Reactivate Trauma Memories
Smells, sounds, places, or emotional states can activate trauma memory networks. When this happens:
-
Stress hormones spike
-
Anxiety or dissociation increases
-
Cravings emerge as a learned coping response
Image caption: Trauma triggers activate stress responses that intensify urges to self-soothe through substances.
The Role of Hyperarousal and Dissociation
PTSD often swings between two extremes:
-
Hyperarousal: panic, agitation, insomnia, irritability
-
Dissociation: emotional numbness, detachment, emptiness
Substances may be used to:
-
Slow down an overstimulated nervous system
-
Feel something when numb
Cravings are the brain’s attempt to restore balance—albeit in a harmful way.
Why Willpower Alone Isn’t Enough
Cravings rooted in PTSD are not moral failures or lack of discipline. They are neurobiological survival responses.
When trauma is untreated:
-
The brain prioritizes short-term relief
-
Logical reasoning is overridden
-
Relapse risk remains high
This is why traditional addiction treatment often fails without trauma-informed care.
Healing PTSD-Driven Cravings
Effective recovery focuses on treating both trauma and addiction simultaneously.
Trauma-Informed Approaches Include:
-
EMDR (Eye Movement Desensitization and Reprocessing)
-
Somatic therapies to regulate the nervous system
-
Trauma-focused CBT
-
Mindfulness and grounding practices
-
Medication for PTSD symptoms when appropriate
Image caption: Trauma-informed therapies help retrain the brain to manage stress without substances.
A Compassionate Path Forward
When PTSD triggers substance cravings, the goal isn’t just sobriety—it’s safety, regulation, and healing. As trauma is processed and the nervous system stabilizes, cravings often lose their intensity and control.
Recovery becomes sustainable not because urges disappear overnight, but because the brain no longer needs substances to survive.