Local officials are alerting the public to a powerful animal sedative tainting Cincinnati’s illicit drug supply.
The sedative was found in 457 drug seizures in the third quarter of this year, according to data provided by Hamilton County Public Health, a jump from 23 seizures at the end of 2023, our media partners at the Enquirer report.
Medetomidine, also known as “dex”, has been used for years as a veterinary tranquilizer. But as the latest drug being mixed with fentanyl and other substances along the East Coast and in parts of the Midwest, it’s causing people to experience withdrawal so severe that in some cases, treatment requires hospitalization in the ICU. And some people have died.
Dr. Carolyn Chan, an addiction medicine and internal medicine physician at UC Health who treats patients with substance use disorder, said she first started seeing a handful of “unusual” cases about a year ago.
These patients showed withdrawal symptoms that were “a little bit out of proportion” with what she usually encountered with opioid withdrawal. And while treating patients who’ve often been exposed to “a hodgepodge of substances” on the street always involves a degree of uncertainty, Chan said the usual medications prescribed to treat opioid addiction weren’t working.
“They were still getting sick,” said Chan, who’s noticed an uptick of patients within the past couple months with symptoms that she strongly suspects were caused by medetomidine.
Newtown Police Chief Tom Synan said that toxicology reports in two overdose deaths in the Cincinnati area this year showed that medetomidine was the only substance found in their system.
“It’s causing people to go unconscious very quickly, stay unconscious for several hours and then have severe withdrawals,” said Synan. “The people that we talked to who are chronic users, they did not ask for medetomidine.”
What is medetomidine?
Medetomidine is a sedative that’s approved for use in animals, as a veterinarian tool, but not humans. Chan calls it an “emerging adulterant” of the illicit opioid supply.
It is not an opioid, which is why naloxone, the opioid overdose antidote, doesn’t help with the withdrawal that medetomidine causes.
Medetomidine is 100 times to 200 times more powerful than xylazine, the livestock tranquilizer that’s considered its predecessor.
“It has overtaken xylazine as the most common cutting agent,” said Andrea Hatten, chief administrator of Hamilton County Coroner’s Office, in an email to The Enquirer.
Synan said he’s heard that on the street medetomidine is being called “a safer tranq” compared to xylazine, which is known for creating open wounds, skin ulcers and sometimes, devastating necrosis.
“That’s not true,” said Synan. “You may not be getting the wounds, but the withdrawal is severe.”
Chan agrees. “Xylazine rarely needs ICU level-care to treat the withdrawal syndrome,” she said. “Medetomidine withdrawal, sometimes it does.”
How to spot medetomidine
Medetomidine doesn’t have any immediately recognizable physical characteristics that you can see, smell or taste, according to Chan. Nor is there a way for doctors to be able to test a patient for medetomidine when they seek treatment.
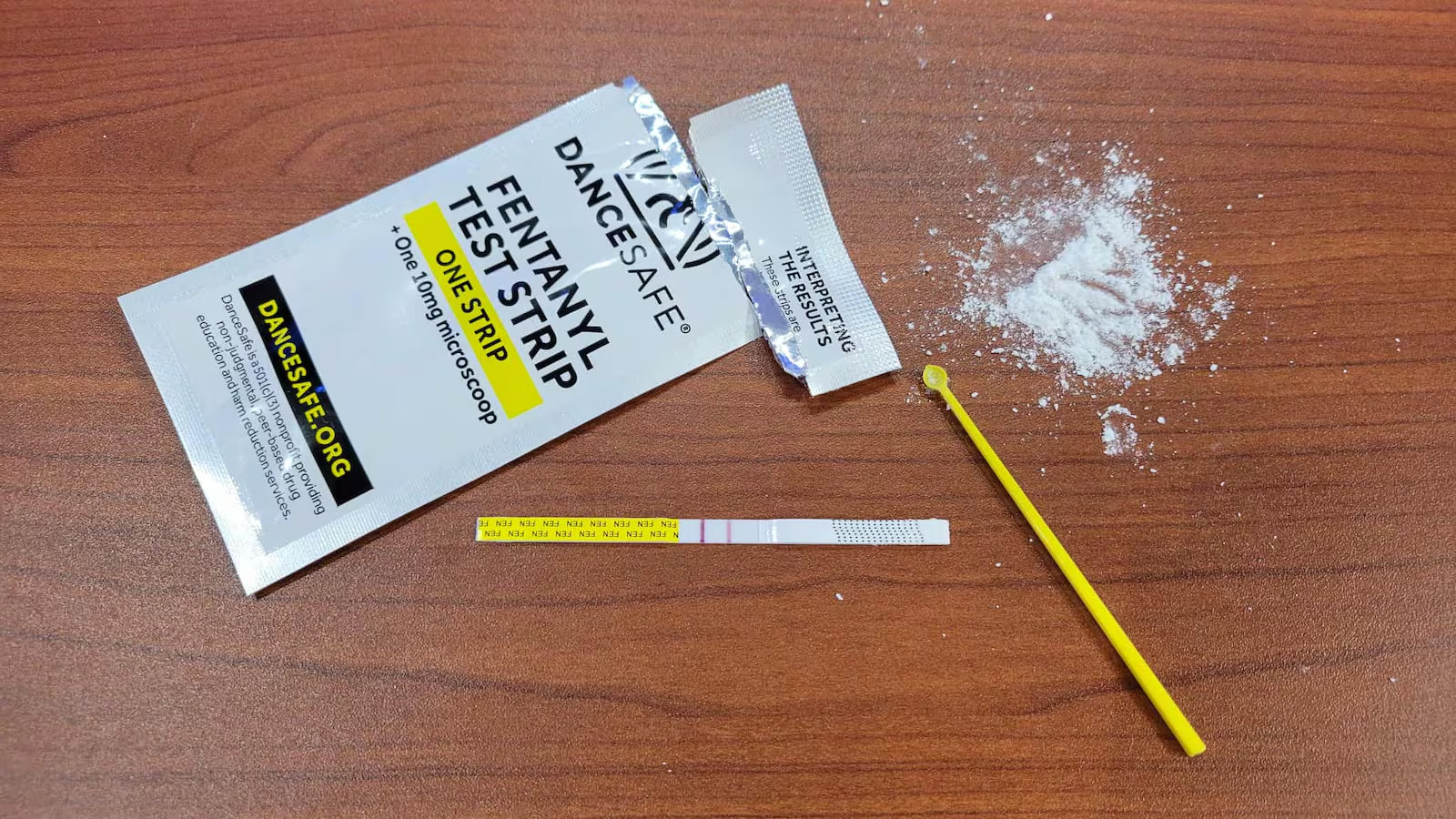
However, patients can get medetomidine testing strips for free at Hamilton County Public Health’s SAFE services locations.
Caracole, an HIV/AIDS services nonprofit that operates as a SAFE services location in Northside, distributes testing strips, too, through its vending machine outside of the building. The vending machine operates 24/7, though patients must enter the building or call (513) 761-1480 to receive an access code.
Chan advises caution when using the strips, which may not always pick up on smaller concentrations of the medetomidine.
“If it’s positive, you definitely want to avoid using it,” she said. “But if it’s negative, I still tell folks be very cautious, because these tests are not slam dunks.”
Symptoms of medetomidine-involved withdrawal or overdose
If you think you or someone you know is going through a medetomidine-involved withdrawal, seek medical care.
“There can be some serious complications for medetomidine withdrawal,” said Chan, including cardiac issues. “Early treatment and identification can help decrease their risk.”
Treating the patient with naloxone is still the first recommended course of action, according to Chan, because the person could also be experiencing a fentanyl overdose.
Symptoms of medetomidine withdrawal, which could also be worsened by the simultaneous effects of fentanyl, include an abnormally high heart rate, high blood pressure, nausea and uncontrollable vomiting that requires some patients to receive IV fluids for dehydration, according to Chan. Muscle aches, cramps and chills are also common.
In severe cases of withdrawal, patients “may be confused” and experience significant tremors.
Treating these patients with medication that is chemically similar to medetomidine can “replace that deficit folks have from withdrawal,” said Chan, and allow them to “improve rapidly.”
Signs of opioid overdose include a slow breath rate, sleepiness, the skin taking on a bluish or ashen tone, and unresponsiveness or difficulty with waking up. If you see these symptoms, call 911 immediately and administer naloxone if it’s available.