Introduction
Many people who struggle with addiction carry trauma that is never formally diagnosed. While severe Post-Traumatic Stress Disorder (PTSD) is widely recognized, mild PTSD often goes unnoticed—especially in individuals battling substance use. Yet even low-grade trauma symptoms can quietly fuel cravings, emotional dysregulation, and relapse. Identifying mild PTSD is a crucial step toward lasting recovery.
What Is Mild PTSD?
Mild PTSD does not always involve vivid flashbacks or debilitating panic attacks. Instead, it often presents as persistent emotional and behavioral patterns that interfere with daily life but may seem “manageable” on the surface.
Common characteristics include:
-
Heightened stress sensitivity
-
Emotional numbness or detachment
-
Irritability or sudden mood shifts
-
Sleep disturbances or vivid dreams
-
Avoidance of reminders linked to past experiences
For individuals with addiction, these symptoms are frequently masked by substance use itself.
Why Mild PTSD Is Common in Addiction
Trauma and addiction are deeply intertwined. Many people turn to substances as a coping mechanism—an attempt to regulate emotions, silence intrusive thoughts, or regain a sense of control.
Key reasons mild PTSD often coexists with addiction:
-
Early life trauma: Emotional neglect, abuse, or unstable environments
-
Chronic stress exposure: Long-term pressure rather than a single traumatic event
-
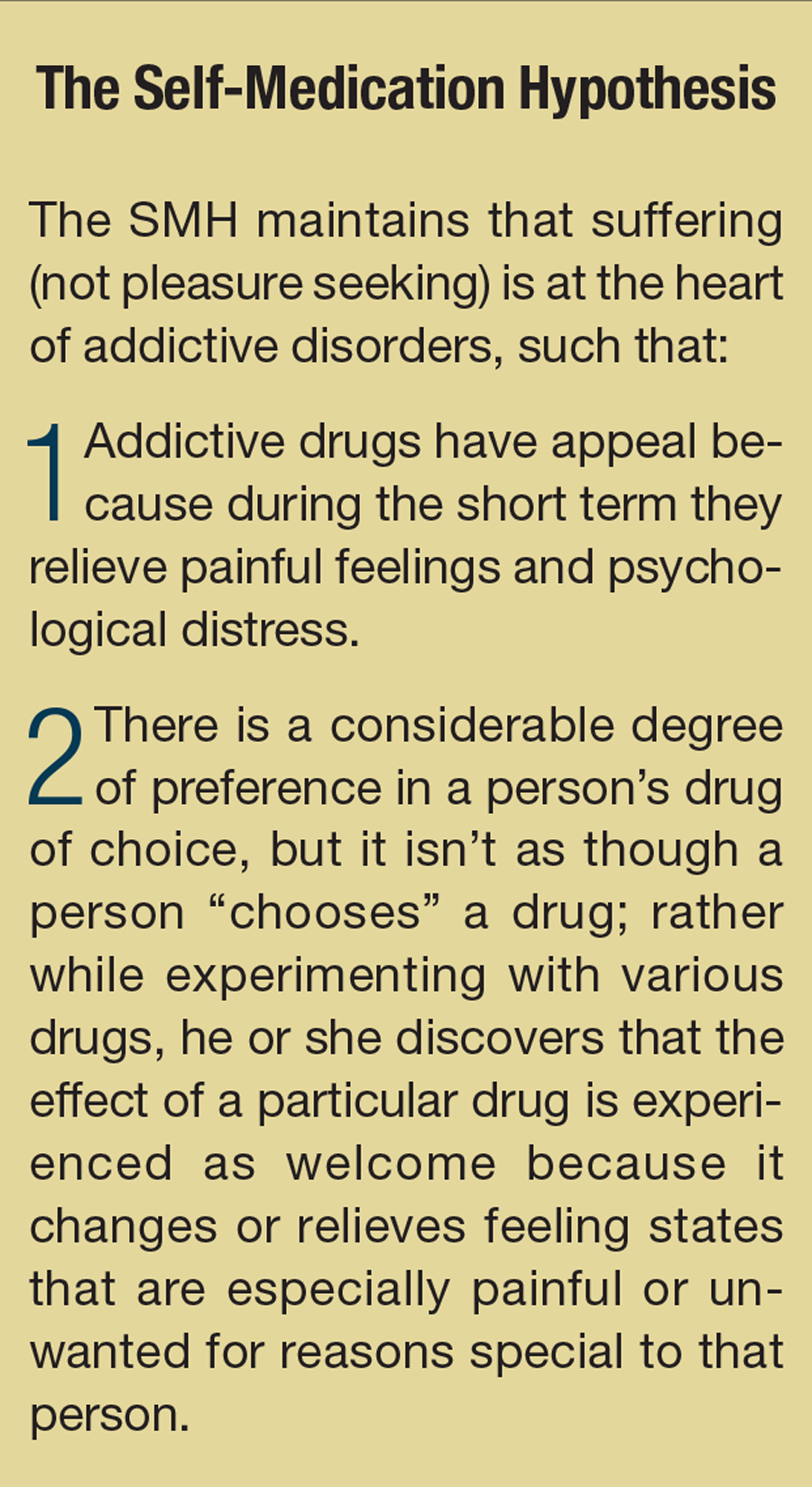
Self-medication: Substances temporarily reduce anxiety or emotional pain
-
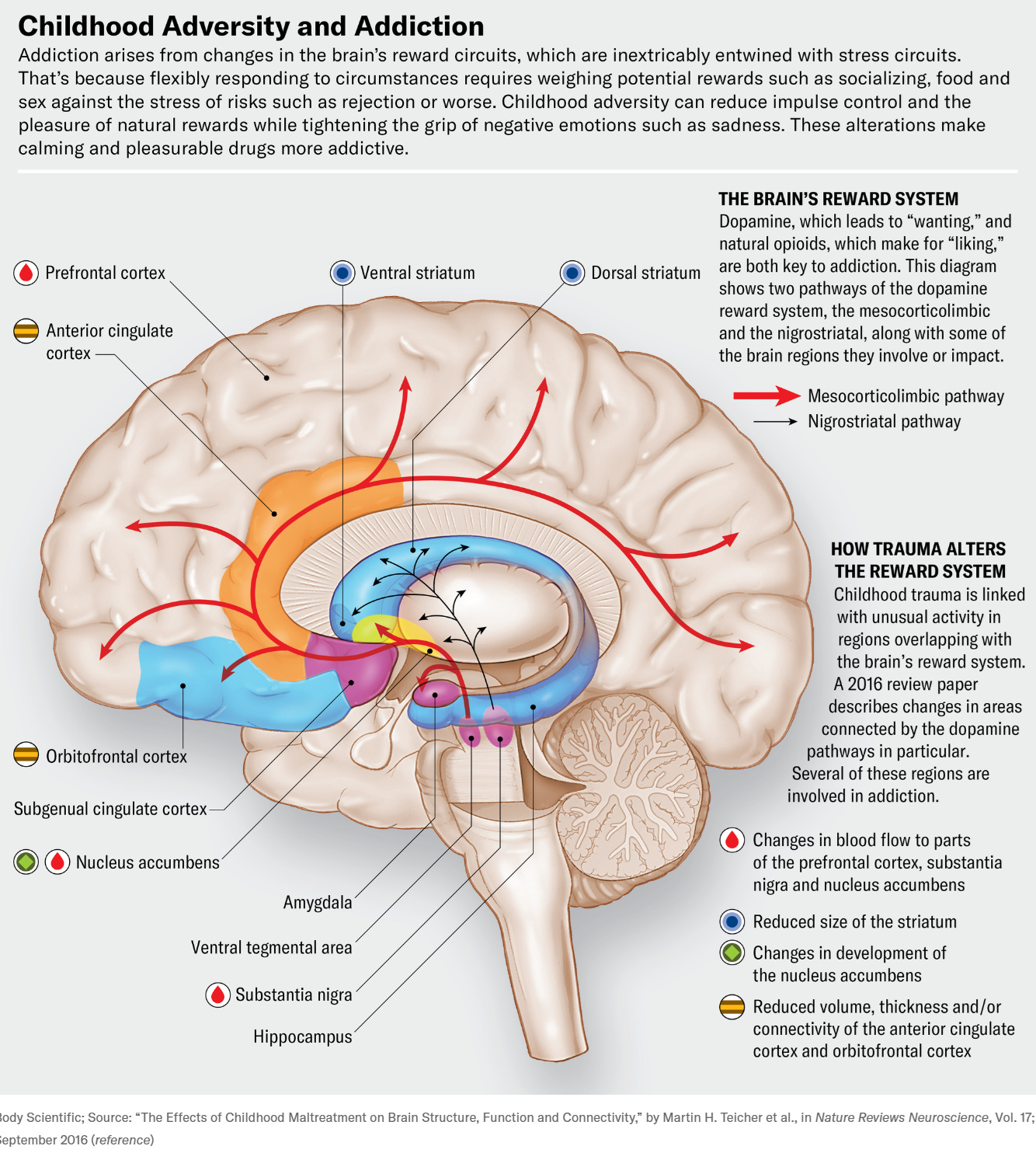
Neurobiological overlap: Trauma and addiction affect the same stress and reward pathways in the brain
Over time, substance use may dull trauma symptoms—but it also prevents true healing.
Signs of Mild PTSD in People With Addiction
Mild PTSD can look very different in someone struggling with substance use. Warning signs may include:
-
Using substances primarily to “feel normal” rather than to feel high
-
Strong emotional reactions to seemingly minor stressors
-
Difficulty relaxing or feeling safe, even in calm environments
-
Persistent guilt, shame, or self-blame
-
Relapse patterns triggered by emotional discomfort rather than cravings alone
These signs are often misattributed to “addictive personality” traits instead of unresolved trauma.
Why It Often Goes Undiagnosed
Mild PTSD is frequently overlooked because:
-
Symptoms are normalized (“I’ve always been this way”)
-
Addiction treatment focuses on behavior, not trauma history
-
Individuals minimize their experiences, believing trauma must be extreme to count
-
Clinicians may prioritize acute withdrawal and relapse prevention
As a result, the root cause remains untreated.
The Importance of Trauma-Informed Recovery
Recovery that ignores trauma is often incomplete. Addressing mild PTSD can significantly improve treatment outcomes.
Effective trauma-informed approaches may include:
-
Trauma-focused CBT: Reframing trauma-linked thought patterns
-
EMDR: Processing unresolved traumatic memories
-
Somatic therapies: Regulating the nervous system through body awareness
-
Mindfulness-based interventions: Increasing emotional tolerance without substances
When trauma is acknowledged, cravings often lose their emotional power.
Healing Beyond Abstinence
Sobriety alone does not resolve trauma. For many, true recovery begins when emotional safety replaces survival mode. Identifying mild PTSD allows individuals to understand why they use—not just that they use.
Healing is not about reliving the past, but about freeing the present from its grip.
Final Thoughts
Mild PTSD may be subtle, but its impact on addiction is profound. Recognizing these hidden trauma patterns can transform recovery from a cycle of relapse into a process of genuine healing. When trauma is treated with compassion and skill, recovery becomes not only possible—but sustainable.