


The Link Between Depression and Alcohol Use
Introduction
Depression and alcohol use are closely intertwined in ways that often deepen suffering rather than relieve it. Many people turn to alcohol in moments of emotional pain, hoping to quiet sadness, numb anxiety, or escape heavy thoughts. While alcohol may offer brief relief, its long-term effects can worsen mood, intensify depressive symptoms, and create a harmful cycle that is difficult to break. Understanding how depression and alcohol use influence each other is a critical step toward healing and recovery.
Why Depression and Alcohol Often Go Hand in Hand
Depression affects how the brain processes pleasure, motivation, and stress. Alcohol temporarily alters brain chemistry, increasing dopamine and relaxing inhibitions, which can feel soothing to someone who is emotionally overwhelmed. For this reason, people experiencing depression may be more likely to use alcohol as a form of self-medication. Over time, however, the brain adapts, requiring more alcohol to achieve the same effect—leading to increased use and dependency.



Image caption: Alcohol may feel calming at first, but it disrupts brain chemistry linked to mood regulation.
How Alcohol Worsens Depressive Symptoms
Although alcohol is often perceived as a mood booster, it is actually a depressant. Regular drinking interferes with neurotransmitters like serotonin and dopamine, both essential for emotional balance. Alcohol also disrupts sleep, increases fatigue, and reduces motivation—core symptoms already common in depression. Over time, this can deepen feelings of hopelessness, guilt, and emotional numbness.



Image caption: Alcohol-related sleep disruption can intensify fatigue and low mood.
The Vicious Cycle: Drinking to Cope, Feeling Worse After
One of the most dangerous aspects of the depression–alcohol connection is the feedback loop it creates. A person drinks to cope with depressive feelings, experiences temporary relief, then feels worse as alcohol wears off. This emotional crash often leads to more drinking, reinforcing both the depression and the reliance on alcohol. Over time, this cycle can escalate into alcohol use disorder alongside worsening mental health.

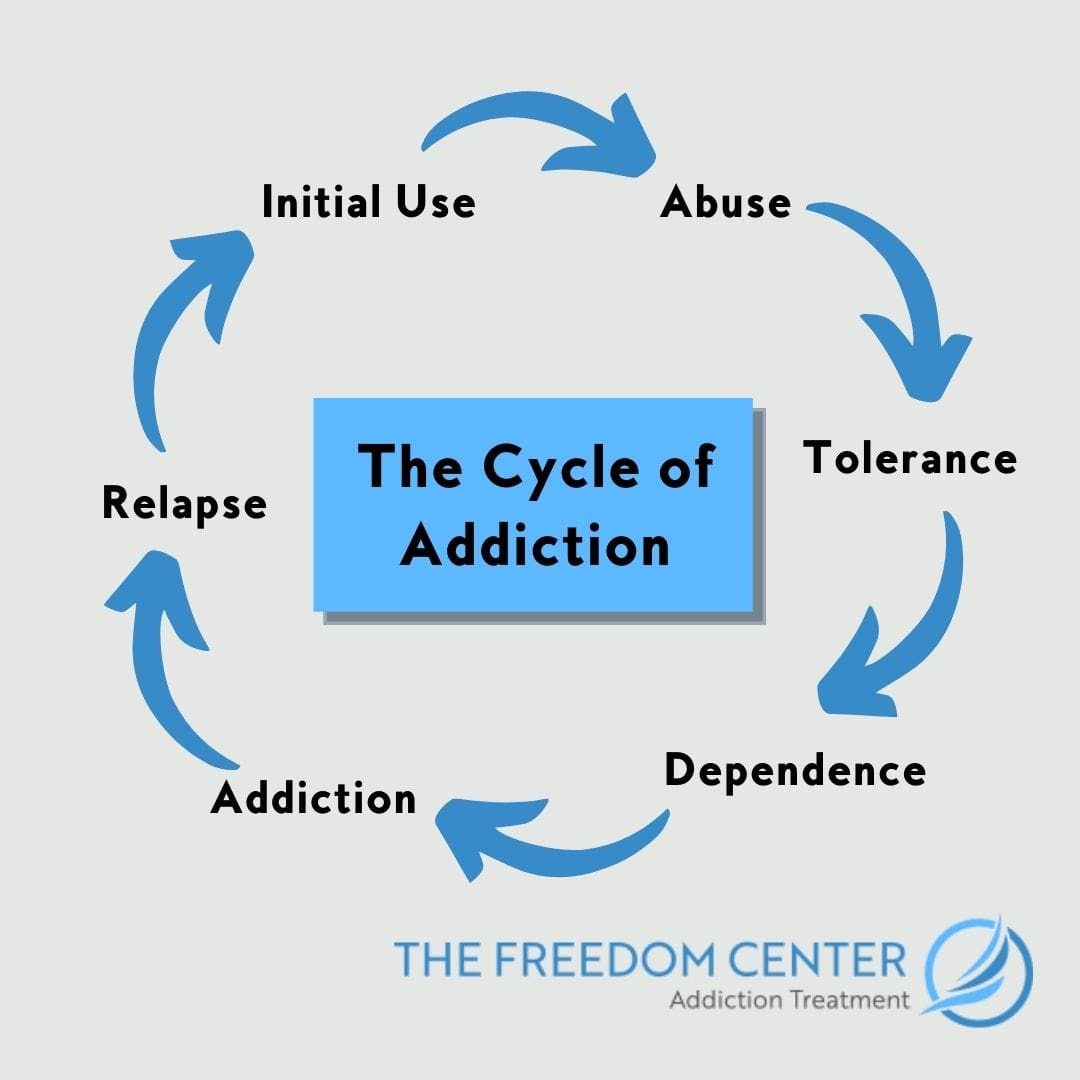

Image caption: Depression and alcohol use often reinforce each other in a repeating cycle.
Risk Factors That Increase Vulnerability
Certain factors make people more vulnerable to developing both depression and problematic alcohol use. These include chronic stress, trauma, social isolation, genetic predisposition, and lack of emotional support. Major life transitions—such as loss, relationship breakdowns, or financial hardship—can also increase the likelihood of turning to alcohol during depressive episodes.
Why Quitting Alcohol Can Improve Mood
Many people are surprised to find that reducing or stopping alcohol use can significantly improve depressive symptoms. Once alcohol is removed, the brain begins to rebalance its natural chemistry, sleep quality improves, and emotional clarity gradually returns. While the early stages of cutting back may feel challenging, long-term emotional stability is often greatly enhanced.



Image caption: Reducing alcohol use can support emotional healing and mental clarity.
Healthy Ways to Cope With Depression Instead of Drinking
Replacing alcohol with healthier coping strategies is essential for recovery. Effective alternatives include therapy, regular physical activity, mindfulness practices, journaling, social connection, and professional mental health support. These approaches address the root causes of depression rather than masking symptoms, leading to more sustainable healing.
When to Seek Professional Help
If depression and alcohol use feel intertwined or difficult to control, professional help is strongly recommended. Mental health professionals can provide integrated treatment that addresses both conditions simultaneously. Seeking support is not a sign of weakness—it is a powerful step toward reclaiming emotional well-being and long-term health.
Conclusion
The link between depression and alcohol use is complex, but it is not unbreakable. Understanding how alcohol affects mood—and recognizing when it becomes a coping mechanism rather than a solution—can open the door to meaningful change. With awareness, support, and healthier coping strategies, it is possible to break the cycle and move toward a more balanced, hopeful life.
