Trauma leaves more than memories — it reshapes the brain, the nervous system, and the way people cope with emotional pain. For many, addiction is not about pleasure or weakness, but about survival. Understanding the deep connection between trauma and addiction is essential for compassion, effective treatment, and long-term recovery.
Understanding Trauma and Its Lasting Impact
Trauma occurs when an experience overwhelms a person’s ability to cope. It can result from childhood abuse, neglect, domestic violence, accidents, loss, war, or chronic emotional stress. When trauma is unresolved, the body and brain remain stuck in survival mode.
Instead of feeling safe, the nervous system stays hyper-alert or emotionally numb. This constant internal tension often drives people to seek relief — and substances can temporarily provide that escape.
Illustration: Emotional distress and hypervigilance commonly seen after traumatic experiences.
How Trauma Changes the Brain
Trauma directly affects brain regions involved in emotion, stress, and decision-making:
-
Amygdala becomes overactive, increasing fear and anxiety
-
Prefrontal cortex weakens, reducing impulse control
-
Hippocampus struggles with memory and emotional regulation
At the same time, trauma disrupts the brain’s dopamine system — the same system involved in addiction. This makes substances feel unusually relieving, reinforcing repeated use.
Illustration: Trauma alters brain circuits linked to fear, reward, and impulse control.
Addiction as a Coping Mechanism
For many trauma survivors, substances serve a purpose:
-
Alcohol may quiet intrusive memories
-
Drugs may numb emotional pain
-
Nicotine may regulate anxiety
-
Stimulants may counter emotional numbness
This process is known as self-medication. The relief is real — but temporary. Over time, tolerance grows, dependence forms, and addiction takes hold.
What begins as a coping strategy slowly becomes another source of trauma.
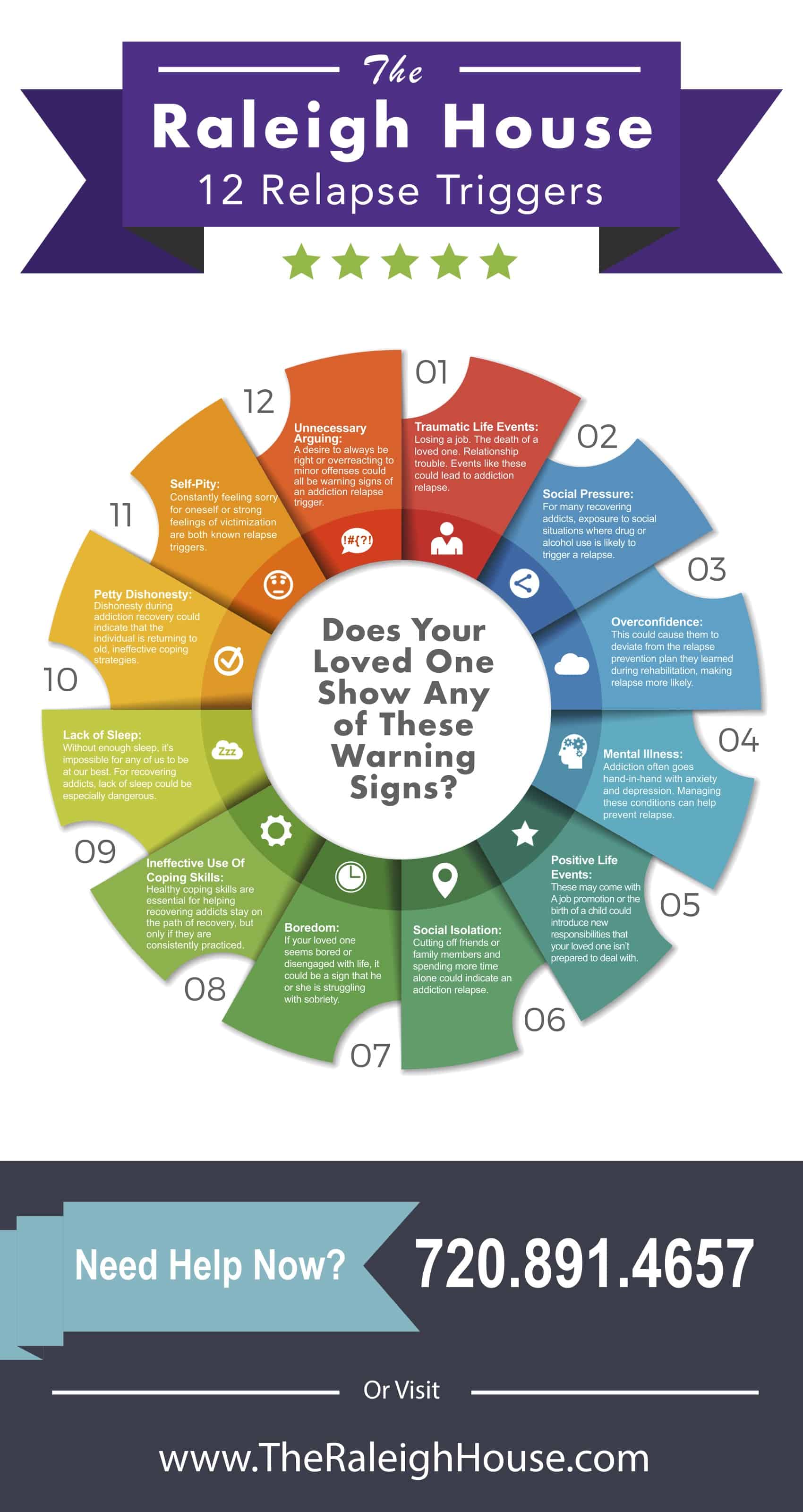
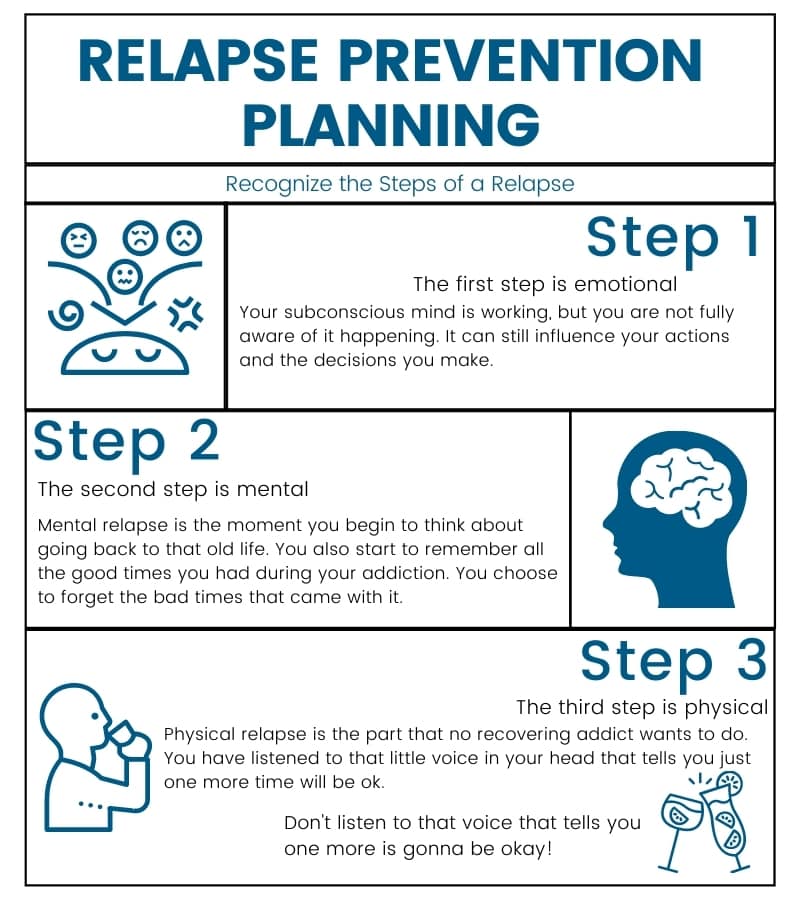
Why Trauma Increases Relapse Risk
Even after detox or treatment, unresolved trauma remains a powerful relapse trigger. Stress, conflict, or reminders of past trauma can activate the nervous system instantly — long before rational thinking kicks in.
Without trauma-informed support, relapse is not a failure of willpower. It is the brain returning to a learned survival response.
Illustration: Stress and emotional triggers can reactivate trauma-driven cravings.
The Trauma–Addiction Cycle
-
Trauma causes emotional pain
-
Substances provide short-term relief
-
Dependence and addiction develop
-
Shame and consequences deepen trauma
-
The cycle repeats
Breaking this cycle requires addressing both addiction and trauma — not one without the other.
Healing Requires Trauma-Informed Recovery
Effective recovery for trauma-affected individuals includes:
-
Trauma-informed therapy (EMDR, somatic therapy, trauma-focused CBT)
-
Nervous system regulation skills
-
Safe, supportive relationships
-
Gradual rebuilding of trust and self-compassion
Recovery is not about erasing the past — it’s about teaching the brain that safety is possible again without substances.